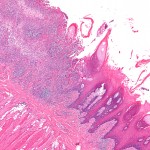
Oral leukoplakia is the commonest of the oral potential malignant disorders (OPMDs) with a prevalence of 2.6% (95%CI; 1.72-2.74). A proportion of oral leukoplakia undergo malignant transformation with rates between 0-20% having been reported. The aim of this review was to ascertain the malignant transformation rate of oral leukoplakia (OL) and the associated risk factors.
Methods
Searches were conducted in the Medline/PubMed and Embase databases. Prospective or retrospective cohort studies were considered. Studies describing the pre-leukoplakia, proliferative verrucous leukoplakia and snuff-induced lesions were excluded as were studies reporting the same cohort at different time points. A narrative summary of the included studies and summary data are presented.
Results
- 24 studies involving a total of 12,103 patients were included.
- A majority (14) of the studies were retrospective.
- Studies from 13 countries were included Sweden, Denmark, India, Hungary, UK, USA, Norway, Japan, Netherlands, Taiwan, Italy, Croatia and China.
- The range of malignant transformation was between 0.13% and 34.0%.
- The mean rate of transformation among all studies in patients with OL was 14.9%
- 3 studies calculated a specific annual transformation for OL. The range was 0.3% to 6.9% with a mean of 3.8% per year with a range of follow-up time 2.4–11 years.
- Only 11 studies reported the site of malignant transformation with only 6 indicating the number of cases per original sites of leukoplakia, which transformed into cancer. Buccal mucosa was the commonest site in these studies but had the lowest rate of transformation (3.53%), while tongue (24.22%) and tongue and floor of mouth (14.85%) had the highest rates of transformation.
- Features that stood out as significant determinants contributing to malignant potential of OL included
- Advanced age,
- Female sex,
- Leukoplakia exceeding 200 mm2,
- Non-homogeneous type (e.g. erythroleukoplakia) and the higher grades of dysplasia.
Conclusions
The authors concluded: –
Malignant transformation rate of OL varies from 0.13 to 34% across the 24 studies reviewed here. Age, gender, clinical type of the lesion and the grade of dysplasia were found to be important risk factors for malignant transformation.
Advancing age was found to be an important risk factor. Due to the heterogeneity of the age group classification across the reviewed studies, it was difficult to derive a conclusion on the involvement of age as a risk factor. Although OL is relatively uncommon among females compared to males, the malignant transformation was found to be significantly higher among females. Non-homogenous leukoplakia was found to have a higher risk in malignant transformation. In three studies, the dysplasia grade did influence the risk for transformation. It is imperative for clinicians to have more evidence-based information to make sound decisions in clinical management of OL. For the reasons discussed, more studies with clear case definitions are required.
Comments
The reviews search was limited to only two major databases and the English language, so it is likely that relevant studies were not identified. While studies were screened by both authors for inclusion, it is not clear whether this was carried out independently. In addition, the quality of the included studies does not appear to have been assessed. Key findings from each of the included studies are provided in a narrative study and no formal pooling of the studies has been conducted with simple summary statistics provided. The authors note that annual transformation rate is an important guide for clinical practice but note that most studies did not report this or provide enough information for it to be calculated. Challenges also exist because of the use of difference criteria. As the authors note better reported higher quality studies with clear case definitions are needed to inform clinical decisions.
Links
Warnakulasuriya S, Ariyawardana A. Malignant transformation of oral leukoplakia: a systematic review of observational studies. J Oral Pathol Med. 2015 Jul 20. doi: 10.1111/jop.12339. [Epub ahead of print] PubMed PMID: 26189354.
Lodi G, Sardella A, Bez C, Demarosi F, Carrassi A. Interventions for treating oral leukoplakia. Cochrane Database of Systematic Reviews 2006, Issue 4. Art. No.: CD001829. DOI: 10.1002/14651858.CD001829.pub3.

Malignant transformation of oral leukoplakia http://t.co/a8MQrF6rKy
Oral Leukoplakia has variable malignant transformation rate http://t.co/a8MQrF6rKy
Malignant transformation of oral leukoplakia varies http://t.co/a8MQrFo2C6
Oral Leukoplakia: malignant transformation rate varies http://t.co/a8MQrF6rKy
Don’t miss – Oral Leukoplakia: malignant transformation rate highly variable http://t.co/a8MQrF6rKy
[…] Dental Elf – 24th July 2015 – Oral leukoplakia: malignant transformation rate highly var… […]